Designing a Healthcare Platform for Longitudinal Care
OVERVIEW
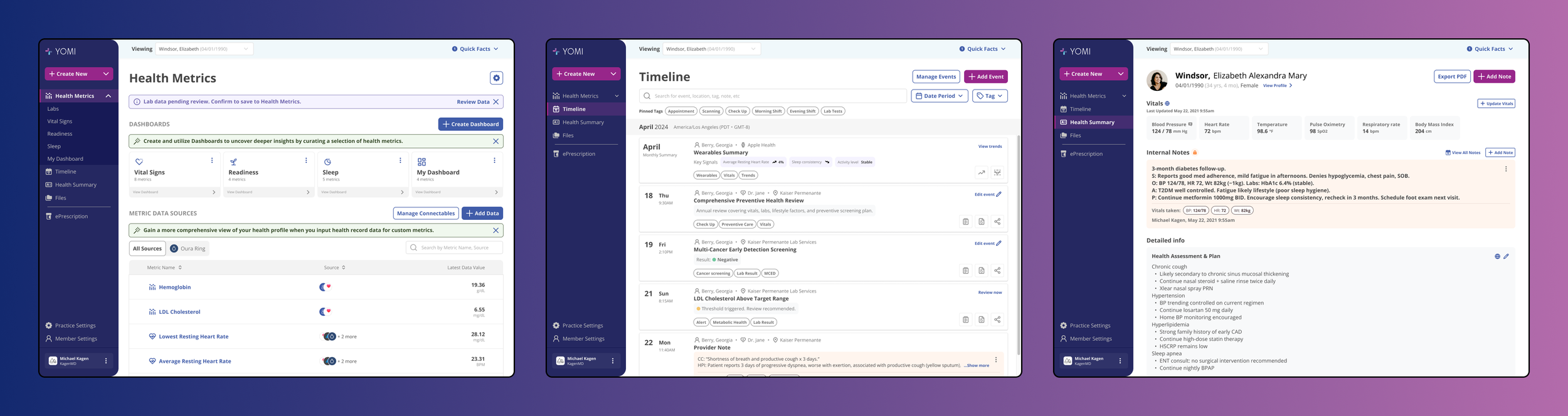
YOMI Health is a healthcare platform designed to support concierge medical practices by replacing fragmented, encounter-based workflows with a longitudinal, system-of-record approach to patient health.
I lead product and design for YOMI Health end-to-end as a fractional UX lead, working closely with the founder and clinical staff. Unlike traditional UX engagements, this work extends beyond interface design into product definition, domain modeling, and strategic decision-making. The platform is actively used by a real medical practice to manage patients, monitor health data, and support clinical decisions.
This case study focuses on how the product evolved strategically in response to real-world constraints, clinical needs, and market realities, rather than on feature-by-feature execution. The scope and nature of my involvement evolved over time, from hands-on execution to product direction, prioritization, and design leadership across the system.
CONTEXT & CONSTRAINTS
Concierge medicine operates very differently from traditional healthcare systems.
Key constraints included:
No insurance billing workflows
High-touch, long-term patient relationships
Emphasis on prevention, monitoring, and early intervention
Heavy reliance on external data sources such as labs and wearables
Clinicians managing complex histories across long time horizons
Existing EMRs are optimized for billing and episodic encounters. They fragment patient history, bury signal in documentation, and require clinicians to reconstruct context manually.
YOMI Health’s challenge was not to “modernize an EMR UI,” but to redefine what the system should represent in the first place.
PROBLEM FRAMING
Early exploration revealed that the core issue was conceptual, not visual.
Traditional systems treat healthcare as a sequence of encounters. Concierge medicine treats healthcare as an ongoing relationship.
This raised foundational questions:
What is the primary unit of health information?
How should clinical history be represented over time?
How do clinicians detect meaningful change across months or years?
How do you reduce cognitive load without losing clinical rigor?
Answering these required product decisions before any interface decisions could be made.
STRATEGIC DECISIONS MADE
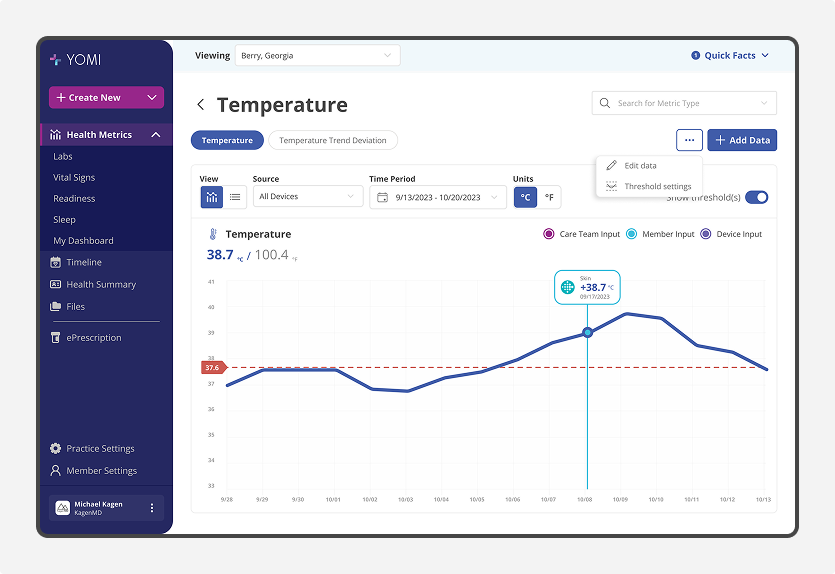
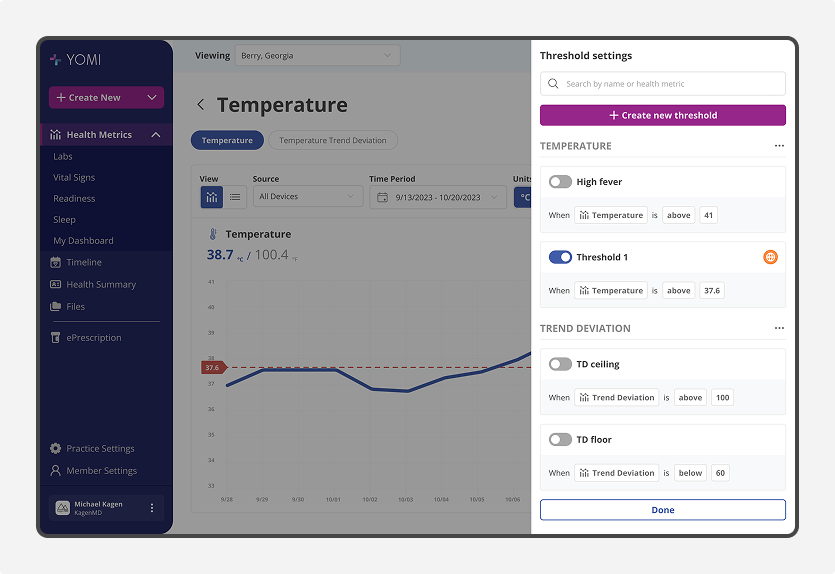
Designing for Decision Enablement
YOMI Health is designed to actively support clinical judgment. Rather than functioning as a system of record, the product is built to help clinicians reason under time pressure, uncertainty, and real-world constriants.
Deviation surfaced without manual analysis.
Key design decisions included:
Threshold-based alerts on wearable and lab data
Emphasizing trends and change over raw values
Surfacing abnormal or shifting metrics early
Enabling clinicians to quickly reconstruct context before patient interactions
Success is measured not by clicks, but by confidence and speed of clinical reasoning.
Redefining the Core Data Model: Health Events Over Encounters
One of the earliest and most consequential decisions was to abandon the concept of “encounters” as the organizing principle.
A single event model supporting multiple clinical realities
Instead, I defined health events as the core unit of the system. Events can represent:
Lab results
Wearable milestones
Clinical observations and notes
Screenings and procedures
Alerts, thresholds, and interventions
This reframed health as a continuous narrative rather than a series of disconnected visits.
That decision enabled:
Longitudinal visibility across domains
Pattern recognition over time
Preservation of clinical context
A shared mental model across care teams
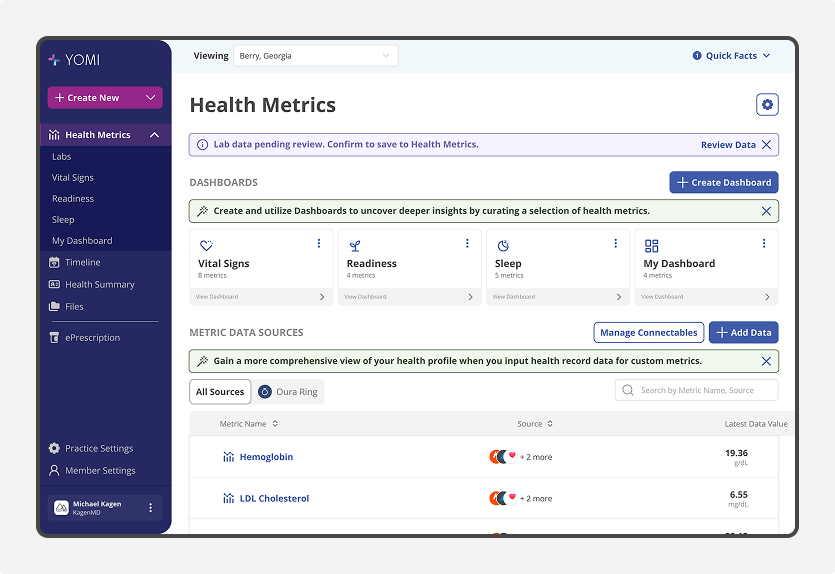
Once health events became the core data model, a chronological representation was no longer optional.
Timeline as the Primary Interface
The timeline is not a feature. It is the direct expression of the event-based model.
Because all health information is structured as events, the most natural and clinically meaningful way to access that information is through a timeline. The timeline aggregates heterogeneous data sources, surfaces clinically relevant moments, and preserves narrative continuity across time.
It also supports filtering by health domains, such as cancer screening or metabolic health, allowing clinicians to focus without losing broader context.
Designing the timeline required careful trade-offs between density and readability. Clinicians consistently favored information-rich views over minimalism, so the design intentionally prioritizes completeness and signal over visual simplicity.
Designing Health Metrics for Longitudinal Decision-Making
As part of a broader focus on decision enablement, clinicians rely heavily on quantitative signals to understand how a patient’s health is evolving over time.
I designed YOMI Health’s Health Metrics as a longitudinal system rather than a collection of isolated values. Metrics are contextualized through trends, baselines, and clinically meaningful thresholds, allowing clinicians to distinguish normal variation from meaningful change at a glance.
Health Metrics are designed to complement, not compete with, narrative documentation. They provide quantitative grounding for clinical decisions while remaining connected to encounters, notes, and outcomes elsewhere in the system. This reduces cognitive load and avoids forcing clinicians to switch mental models.
Because different clinicians prioritize different signals, the system supports flexibility in which metrics are emphasized and how they are interpreted. A concierge physician monitoring metabolic health, a specialist reviewing labs, or an athletic-focused practice tracking performance indicators can each focus on what matters most without unnecessary noise.
By treating Health Metrics as a first-class system, the design supports proactive monitoring, early detection of change, and more informed clinical decision-making over time.
Designing a Living, Modular Health Summary
Traditional health summaries are static documents that become outdated almost immediately.
I designed YOMI Health’s Health Summary as a living artifact. It is the primary surface where clinicians actively record, curate, and update a patient’s health information over time while preserving historical context. Rather than capturing a moment, it provides an always-current snapshot that can be quickly understood by anyone accessing it.
A core design decision was to avoid a fixed or standardized template. Instead, the Health Summary is built as a modular system of building blocks, allowing clinicians to construct summaries based on both patient needs and clinical specialization. A radiologist, pediatrician, athletic trainer, or concierge physician can each assemble a summary that reflects the domains most relevant to their practice.
The Health Summary is composed from modular building blocks rather than a fixed template. Different practices assemble summaries based on clinical focus and context, allowing the same system to support concierge care, wellness programs, and athletic performance without redesign.
Because it is modular, the Health Summary can evolve as a patient’s circumstances change. A pregnancy-focused summary might emphasize prenatal milestones, labs, imaging, and trimester-specific notes, while an athlete’s summary could prioritize performance metrics, recovery indicators, and injury history. Sections can be added, updated, or reorganized without losing continuity.
The design also challenges healthcare’s outdated information-sharing norms. In an industry where faxing remains common, YOMI Health’s Health Summary supports controlled, secure online access, allowing care teams to selectively share patient information with external providers and partners. When needed, the same summary can be exported as a PDF without breaking context.
By treating the Health Summary as a living, clinician-curated system rather than a static document, the design reframes documentation as an active tool for shared understanding, collaboration, and long-term care continuity.
This reframed documentation from a clerical task into a byproduct of good system design.
Enabling shared clinical awareness across care teams
Concierge care involves multiple staff members interacting with the same patients.
I designed shared activity surfaces that make actions and updates visible across the care team without requiring explicit task creation for routine work. This reflects real clinical workflows, where follow-up often happens offline, but shared awareness is critical.
By prioritizing visibility over task management, the system supports coordination without introducing unnecessary overhead or process friction.
PRODUCT EVOLUTION THROUGH REAL-WORLD USE
YOMI Health is not a speculative concept. It is used daily by a concierge medical practice.
Because of this, product evolution has been driven by:
Real patient data
Live clinical workflows
Time pressure and accountability
Feedback from physicians and staff
The product has evolved through multiple pivots, particularly as we refined positioning for fundraising and broader market adoption. In my role as acting design lead, I have actively supported investor pitches, demos, and narrative reframing to align the product with market expectations without compromising its core principles.
OUTCOMES & MEASURES OF SUCCESS
Traditional SaaS metrics are not appropriate for YOMI Health’s stage or domain. Instead, success is measured through dependency, replacement, and decision enablement.
Notable indicators include:
YOMI Health functions as the system of record for the practice
Core workflows cannot be performed without it
It replaces a patchwork of spreadsheets, PDFs, and manual tracking
Clinicians rely on it to prepare for patient interactions
It serves as the primary demo artifact in investor and customer pitches
These are strong signals of product viability in a high-risk domain.
INDUSTRY PERSPECTIVE
Third-party recognition further illustrates YOMI’s relevance in the domain. In 2025, Dr. Hillary Lin, MD — a board-certified physician specializing in longevity and concierge care — independently listed YOMI among the “Top 8 Longevity and Concierge Medicine Health Data Management Platforms,” highlighting its distinction in an emerging category of clinical tools.
The core innovation here is the timeline view — instead of trying to cram everything into traditional EMR formats, YOMI organizes everything around a chronological view of patient events.
YOMI proves that focused design trumps feature bloat, delivering a streamlined experience that’s particularly valuable for membership-based practices.
— Hillary Lin, MD, “Top Longevity & Concierge Medicine Platforms (2025)”
CLIENT PERSPECTIVE
This work is conducted in close partnership with the physician running the practice, where trust, consistency, and execution quality are critical given real clinical usage.
“Over two years of collaboration, Bryan has consistently delivered stunning and user-friendly designs. I’ve greatly appreciated his attention to detail, innovation, and commitment to perfection.”
TRADEOFFS & ONGOING TENSIONS
Several tensions remain active:
Balancing information density with usability
Designing for clinicians while preparing for non-clinical buyers
Maintaining product integrity while adapting to market narratives
Building scalable foundations without over-engineering early
These are not problems to “solve,” but constraints to navigate deliberately.
REFLECTION
YOMI Health has reinforced a core belief in my practice: senior design work is often about defining what the product is, not how it looks.
In complex domains, design decisions shape data models, workflows, and mental models long before they shape interfaces. The most impactful work happens upstream, where trade-offs are hardest to see and easiest to get wrong.
Operating in that space requires judgment and the ability to align stakeholders around a shared understanding of intent, especially when constraints are real and outcomes matter.
This way of working did not begin with YOMI Health. In prior work, partners described my impact in similar terms:
“He defined the UX strategy to align the highest standards with all stakeholders by working backwards from user experience.”
At YOMI Health, this translated into operating as an acting and fractional UX lead. While supporting ongoing delivery, I was accountable for defining system architecture, prioritization trade-offs, and the long-term coherence of the product as it moved from concept into active clinical use.
As the platform matured, my role increasingly shifted from hands-on execution toward guiding design direction, prioritization, and system coherence, ensuring the product could scale beyond its initial implementation.